
Subscribe
Data delivered to your inbox. Keep up with the latest developments.How shortages are putting lives in danger across Africa.
This story was originally published on The Guardian Nigeria, as written by Adaugo Trinitas Onyebuchi.
“We rarely sleep”; “we constantly monitor patients on ventilators in the intensive unit, attend to emergencies, take samples, and check on stable patients three times daily”; “the possibility of getting infected is always in my consciousness, I know it can happen, so I tend to be more careful. It is more of a conscious reality than fear”; “I know that each day, my life is on the line. I know it every day that I go out, but I am not afraid” narrates healthcare workers at the LUTH isolation center, according to a report by Tessy Igomu. For many of us, leaving our homes is now accompanied by the fear of being exposed to the Coronavirus (Covid-19). It is even harder to now imagine the anxiety felt by the healthcare workers, who are at the frontline of the Covid-19 pandemic, and the pressure on them to protect themselves from being infected with the virus.
Since the outbreak of Covid-19, which was first reported to the WHO country office in China on the 31st of December 2019 and declared a public health emergency of concern on the 30th of January 2020, there has been an increasing demand on health care services. It has also placed more responsibilities on health care workers and has increased the demand for Personal Protective Equipments (PPE) around the world. Every day, thousands of Covid-19 cases are reported in Africa and across the World. On June 5, Africa reported a total of 169,646 confirmed Covid-19 cases with 90,993 active cases. Therefore, healthcare workers are working tirelessly attending to Covid-19 patients and are hence dependent on PPE to lower their risk of infection.
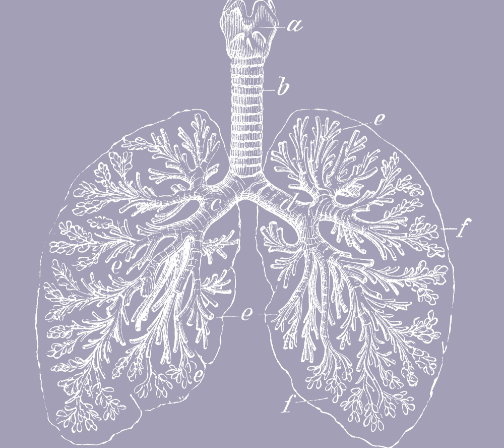
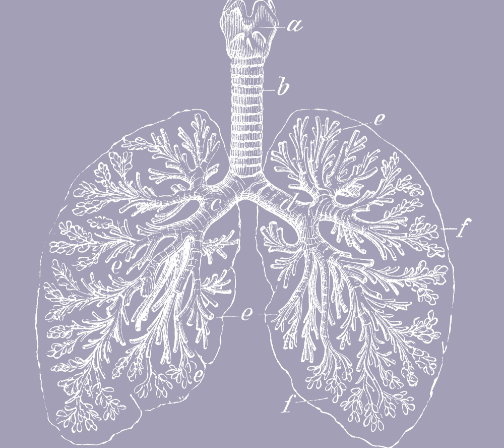
According to WHO, healthcare workers, including doctors, nurses, and community health agents, responsible for protecting the health of their community, should use contact and droplet precaution. This should be done by wearing PPEs such as disposable gloves to protect hands; clean, non-sterile, long-sleeve gown to protect clothes from contamination; medical masks to protect nose and mouth; and eye protection (e.g., goggles, face shield) when attending to COVID-19 patients and should have an in-depth understanding of how to use them. For example, WHO recommends that “Health care workers collecting Nasopharyngeal (NP) and Oropharyngeal (OP) swab specimens from suspected or confirmed Covid-19 patients should be well-trained on the procedure and should wear a clean, non-sterile, long-sleeve gown, a medical mask, eye protection (i.e., goggles or face shield), and gloves. The procedure should be conducted in a separate/isolation room, and during NP specimen collection, health care workers should request the patients to cover their mouth with a medical mask or tissue”.
Unfortunately, the demand for PPE now exceeds supply, endangering the lives of healthcare workers. In March 2020, WHO shipped half a million sets of PPE to 47 countries but supply was still insufficient. In the first quarter of 2020, over 6.4 million gloves, 1 million gowns, and 1.8 million surgical masks were delivered by the United Nations across the world. Nevertheless, the gap between supply and demand is still enormous. Each month, an estimated 89 million medical masks are required for the Covid-19 response. Hoarding, panic buying, and misuse of PPE have contributed to the shortage in its supply, globally.
Healthcare workers in Africa are also at risk as a result of these shortages in PPE and as the number of cases rises, it still remains a major source of concern. According to SABC News, nurses in South Africa are concerned about their exposure to the virus as they do not have adequate access to PPE. In the report, a nurse laments, “I am very afraid because we don’t have any masks, they promised us they will come but meanwhile we are working unprotected and the community still comes in numbers to the clinic. The challenges are lack of protective gear and the government hasn’t conducted training, we haven’t gone for training on how to deal with the coronavirus”.
In April, IOL reported that Lekhoathi, the general secretary of the Democratic Nursing Organisation of South Africa (Denosa), lamented that, “the shortage of PPE is a nightmare to Nurses”.
Dr. Ruth Mary Namyalo, a pharmacist in Uganda, explained that “transportation challenges, caused by the lockdown, have limited their access to PPE. The National Medical stores which supply government-aided facilities have a warehouse in the central business district and no regional stores throughout the country so all facilities have to rely on delivery from the main warehouse”. She added that “before the Covid-19 situation, there wasn’t a single production facility for face masks in Uganda, so we had to rely on imports and since almost the entire world was in lockdown it took time to have them delivered to the country and due to its high demand, we were disadvantaged”.
According to UNICEF, the need for PPE may reach 2.2 billion surgical masks, 13 million goggles, 1.1 billion gloves, and 8.8 million face shields through the end of the year 2020. In addition, as the lockdown is relaxed across Africa, there is a hike in the number of cases, thereby increasing the exposure of healthcare workers, without PPE, to the infection.
In Africa, there are over 2 million doctors, nurses, pharmacists, and community healthcare workers with nursing personnel accounting for 60% of all the healthcare workers. In Nigeria, Uganda, and South Africa alone there are about 370,000 plus healthcare workers including doctors, nurses, pharmacists, and laboratory scientists. Nigeria and South Africa have a strong network of about 116,454 and 51,616 community health agents respectively. In Nigeria, these community workers have also been on the frontline of fighting Covid-19, going door to door to educate families about Covid-19 and to detect and report early symptoms of Covid-19 in the communities. Their efforts have led to an increase in healthy practices, such as hand washing and social distancing in northern communities. However, their families are concerned about their exposure and safety. As the cases rise, these healthcare workers, without adequate access to PPE will be exposed to Covid-19 infection.
In Africa, assuming each current active 90,993 (June 5) Covid-19 patient/case requires medical care and should be attended to by an average of 6 healthcare workers per day, the continent would have a compulsory daily need for at least 545,958 PPE kits including face shields, goggles, apron, medical masks, and gloves. However, due to limited local capacity to ramp up PPE production, and the current supply and demand dynamics including hoarding, misuse, and panic buying, the continent is not meeting the demand for PPE by its health sector.
There is, therefore, an urgent need for the stakeholders in the public and private sectors to collaborate to meet the rising demand for PPE. It is time for Africa to look inwards to increase its local PPE supply. There is an untapped potential of local producers in African countries with the capacity to ramp up PPE supply in the continent. Currently, China is the largest producer of finished products of PPE including its raw materials, followed by Taiwan. Before the pandemic, China and Taiwan were respectively responsible for about 50% and 20% of the supply of surgical/face masks globally. However, with the pandemic, travel, import and export restrictions, the movement of goods across countries and continents have been affected.
Recommendations to Increase Access to PPE
In order to boost local production, the government should incentivize local manufacturing companies to increase their production. Tailors may be supported with grants to increase their capacity to make face masks, aprons, and hospital gowns. According to CNN, Queen Duruibe, a tailor in Aba, produces over 10,000 hypoallergenic face masks a day using cotton and polypropylene, leveraging funding support from Abia state government.
In an interview with Ugochi Obidiegwu, a health and safety consultant, she highlighted that “we have majorly relied on importation to get PPE from other countries, most especially China. With the restriction of travel in this pandemic, it affected the availability, and PPE is really important for our frontline workers”. She also highlighted that “stakeholders must support and patronize local production. Artisans in Aba have over the past few months worked hard to produce various types of PPE to support medical personnel. This should be encouraged”.
Aba, an Eastern Nigeria city, home to 1,078,495 people, has a popular market known as Ariara international market, which is known for its local manufacturing capacity. This market will be a good resource for ramping up the production of PPE in Nigeria and for other African countries. Investors may partner with major manufacturers in the market to train more workers, purchase more equipment, to produce more face masks, aprons, hospital gowns, and hand gloves, for healthcare workers.
African National leaders may also ease interstate movement, export, and import restriction to support the distribution of PPE across states and countries.
More so, non-governmental organizations, including philanthropies and foundations should support manufacturing companies to increase their production by 40 percent as recommended by WHO. This support may be in the form of equipment donation, subsidy for power supply, and financing to increase their access to raw materials.
In addition, healthcare workers, both in urban and rural health facilities, must be trained to understand how to use PPEs. Government bodies through policies should institute mandatory health and safety education covering how to use PPE, highlighting best practices during testing for or attending to Covid-19 patients. Health facilities should be mandated to have toolbox meetings, a common practice that reinforces safety and health standards amongst a group of workers, to provide timely health and safety reminders to healthcare workers.
Health facilities should adopt the WHO’s recommended guidelines for maximizing the use of PPE. This includes the use of telemedicine to evaluate Covid-19 suspected cases limiting their contact with healthcare facilities; the use of physical barriers at hospital triage areas such as registration desks and the pharmacy collection points; and by restricting healthcare workers from entering the rooms of Covid-19 patient if they are not attending to them.
As outlined by Dr. Tedros Adhanom, WHO director-general, during the WHO media briefing to declare Covid-19 a global pandemic, “this is the first pandemic caused as a result of a coronavirus, it is also the first pandemic that can be controlled”. Therefore, Africa has to put in the best of its ability to control the exposure of its front line workers.
This Outbreak story was produced in partnership with the Pulitzer Center and Code for Africa‘s WanaData women data science initiative.